The N.C. Senate released its budget, and the key Medicaid section starts on page 91. A few highlights and some questions and comments:
- Section 12H.1.(b) stops the movement toward a regionalized “Medicaid ACO reform approach” that was the direction that the Executive branch (NC DHHS) had been moving, and is really back toward the Governors initial plan, which I labelled as ‘unworkable’. But, the phrasing below about full-risk capitated plans and provider led and non provider led plans is quite vague, so might really encompass Medicaid ACOs. I don’t know if the language is trying to be coy, or if they don’t really appreciate the nuance under the labels.
- Section 12H.1.(a) would move Medicaid out of NC DHHS and into an independent agency (first sentence below). The execution of such a move is key, but I actually think this is a pretty good idea.
- Section 12H.1.(a) also has some generalities that are difficult to judge without lots more details. There is *massive* amounts of health policy in lines 16-21
SECTION 12H.1 .(a)It is the intent of the General Assembly to transfer the
14 Medicaid and NC Health Choice programs to a new state entity that will define a new, more
15 successful direction for the programs and that will be able to focus more clearly on the
16 operation of the programs. Specifically, the Medicaid program shall move away from
17 unmanaged fee -for-service towards a system that manages care. To that end, Medicaid shall
18 include all dimensions of care for a recipient through full-risk, provider-led and
19 non-provider-led, capitated health plans. Such full-risk capitated health plans shall include all
20 aspects of care, without exceptions, so that the State will bear only the risk of enrollment
21 numbers and enrollment mix
Several comments:
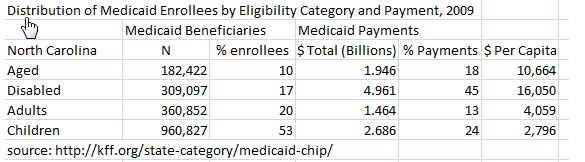
- The paragraph implies that Medicaid is one program, when in reality it is at least 4 programs when viewed in terms of who is covered, what type of care they need, and how much they cost (see below; I know I write this over and over, but it is the most fundamental thing to understand about Medicaid).
For example, the figure below illuminates the “dual eligible” persons, who are covered by Medicare because they are age 65+ typically, and Medicaid because they are poor. They have both acute care needs (doctor, hospital) that are shared by Medicare and Medicaid, and Long Term Care needs (nursing home) that is primarily paid for by Medicaid. There are some children who need nursing home care, for example, but that is very rare for that category of Medicaid beneficiary. And the groups of Medicaid that are the most expensive as shown above (aged, disabled) cost so much because they use lots of acute care as well as Long Term Care. Kids and adults, on the other hand, mostly use acute care.
- The biggest problem with the proposal in lines 17-21-the movement to a completely at risk, capitated system is that it does not make clear what parts of the Medicaid program they intend to do this in? If they mean adults and children-the relatively inexpensive portions of the Medicaid program who mostly need acute care, then it is doable over time. In fact, my white paper is consistent with what they say if that is the patient group focus [I also call for coverage expansion using Medicaid expansion money, but putting beneficiaries into risk based private plans, be they organized by providers or insurance companies].
- If they mean the entire Medicaid program (the aged and disabled, including the dual eligibles as well-the folks who need lots of Long Term Care) will be put totally into an at risk system right away, I don’t think that will work in one of two ways. First way to fail: if you hold a geographical based at-risk system and the price to bid is that you must take all the beneficiaries in an area, then no one is going to bid in at least some parts of the state (or if they do and are for profit, I want to make sure I don’t own their stock). Second way to fail: you break down and say we can’t do it all at once, we will let managed care companies in and bid a subset of the at risk lives, then the insurance companies and perhaps others will cherry pick the best risks (see New York), and later say they need more money or they will leave the state, or stop covering Medicaid. Some of the big health systems might take all comers in certain areas, likely in exchange for Medicaid expansion via a private route (in the language of above, provider led risk plan) or otherwise. However, moving all of the Medicaid program into 100% at risk plans would be one of the biggest health policy changes in the nation’s history. To say more details are needed is an understatement….
- Sections 12.H.3(a) and (b) on page 92 seeks to reduce categorical eligibility and medically needy eligibility criteria for Medicaid beneficiaries who are aged, blind or disabled. The way the Medicaid program works is there are minimums that you must cover, and states can go beyond that if they wish, both in terms of services and eligibility levels (and the federal government pays around two-thirds of the cost in N.C.). This section directs the state to find the lowest eligibility level allowable by law for the elderly, disabled and blind in Medicaid (based on this KFF link, there were ~54,000 medically needy North Carolinians in 2011; total medically needy spending was ~$900 Million in 2011). This would eventually go to zero under the proposal. As a lifelong North Carolinian, I find this section embarrassing.
3.5 years after the Republican Party took over the N.C. General Assembly, all they have are vague generalities on Medicaid reform, except when it comes to running North Carolina to the bottom on coverage for the aged, blind and disabled. We can do better.
a similar post is cross posted at freeforall
You can do pretty well on a capitated system if you simply make it really really hard for expensive people to get care.